Anterior Knee Pain
Anterior knee pain refers to the pain at the anterior aspect of the knee around the knee cap. Prevalence of anterior knee pain is more common in the overweight population, in adolescence and also in the female gender. There is two to seven times more incidence in females than males.
Knee cap is a special type of bone that develops within the tendon of anterior thigh (quadriceps) muscle. It forms a patellofemoral joint along with thigh bone (femur) and moves over the groove (trochlea) of the femur bone. The joint is stabilized by quadriceps muscle specially by its medial fibre (vastus medialis obliques), patellar tendon, medial patellofemoral ligament, retinaculum and other ligamentous bands around it. Knee cap acts as a liver for quadriceps muscle and reduces its energy requirement during knee extension and deceleration. Both are important functions for the activities like walking, running, jogging, squatting, getting up from sitting position, staircase negotiation, uphill or downhill movement.
There are numerous causes of anterior knee pain. It is important to identify and diagnose the exact cause of anterior knee pain for adequate treatment and prevention of further deterioration. Presentation and symptoms of few of these are very much overlapping and thus confusing. Followings are different cause of anterior knee pain.
- Patellofemoral pain syndrome (PFPS) (Hyperlink)
- Chondromalacia patellae (Hyperlink)
- Patellofemoral instability (Hyperlink)
- Isolated osteoarthritis of patellofemoral joint
- Quadriceps tendinopathy
- Osgood-Schlatter disease
- Patellar tendinitis; Jumpers knee
- Prepatellar bursitis; house made’s knee
- Hoffa’s fat pad syndrome
- Plica Syndrome
- Iliotibial band syndrome
- Pes anserine bursitis
Quadriceps Tendinopathy
Quadriceps tendinopathy is a painful condition of the knee presented by activity related to anterior knee pain with localised tenderness at the upper pole of knee cap and muscle tendon area. It is a degenerative condition of the tendon caused by repeated microtrauma of the tendon due to overuse and other related factors.
Quadriceps tendon is the tendinous attachment of anterior thigh muscle with the upper pole of the knee cap. It is the part of the extensor mechanism of the knee which helps in knee extension, bears body weight and stability of the knee joint at different stages of mobilisation. Athletes involving repeated jumping and kneeling activities like basketball and volleyball are at higher risk. Non athletic individuals with high BMI can also develop quadriceps tendinopathy. Hypothyroidism and history of quinolones antibiotics like ciprofloxacin are also considered as risk factors for developing quadriceps tendinopathy.
Symptoms and clinical examination are the keystone of diagnosis. X-ray reveals calcification within tendon and irregular bone formation at upper pole of knee cap. USG and MRI both can detect the condition very effectively. Comparing MRI, USG is cost effective.
Conservative treatment with analgesic, icing, activity modification, proper warm-up and physical therapy is the initial mode of treatment. Physiotherapy in the form of stretching of quadriceps muscle, strengthening of hip and back of the knee muscle is an effective way of reducing stress and strain on quadriceps muscle and letting it heal. Infiltration of affected tendons with PRP helps in its early healing and recovery and is indicated for non-responder of conservative management and high end professional athletes. USG guided infiltration increases the accuracy of infiltration and thus better results. Surgical treatments are reserved for the very late stage of disease with significant degeneration and tear of tendon. It includes debridement of a degenerated tendon with its repair or reconstruction.
Osgood-Schlatter Disease
It is a common painful condition of the knee in adolescence, presented by a painful bony bump at the anterior aspect of shin bone just below the knee joint where the patellar tendon is attached. The area is called tibial tuberosity. It happens in children, especially those who participate in sports activities during their growth spurt. In boys between 12 to14 years and in girls between 10 to 13 years. Intense pain is the early symptom which can aggravate with activity and direct impact. After symptom onset it takes weeks to months to resolve. It usually affects one side but in 20-30% cases it can be bilateral. The condition resolved automatically with the cessation of growth spurt without any residual impact. Very rarely it can be complicated with epiphyseal injury presented as tibial tuberosity avulsion and proximal tibial epiphyseal fracture.
The Bones of children and adolescents have a special area of cartilage which allows it to grow and attach to the muscle tendon. The latter one is called apophysis. Tibial tubercle is an apophysis of patellar tendon. During growth spurt all the bone, cartilage, muscle and tendon passes through rapid changes to accommodate the growth. Repeated strong pull of patellar tendon on its attachment at the tibial tubercle apophysis due to sports activity causes alteration of the cartilage architecture and hampers normal growth and fragmentation of the cartilage. Diagnosis is purely clinical. X-ray, although not mandatory, can revel fragmentation and fluffiness of apophysis.
Rest, icing, analgesic, modification and restriction of sports activity along with stretching and strengthening exercise improves the symptom. It is a self-limiting condition and healed with very minimal residual changes. Sometimes a prominent tibial tuberosity may remain for life long.
Jumper’s knee or Patellar Tendon Tendinitis
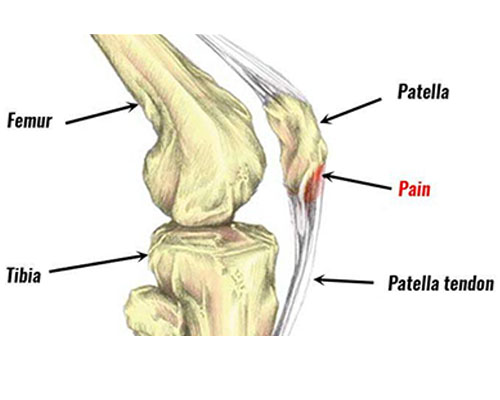
Painful condition of anterior knee with tenderness at inferior pole of knee cap where patellar tendon attached with it. It happens due to repeated microtrauma of patellar tendon due to overstress and lack of recovery time between each trauma. Commonly affects the athlete involved in jumping like volleyball, basketball, high jump and long jump. It can affect non jumping sports like weight lifting, cycling, skiing. Common symptom is pain at the starting of activity and may ease off with continuation of sports during the initial stage of disease. But as disease progresses it affects the performance. In very advanced stages, disruption of the extensor mechanism can happen. Diagnosis is clinically based, x-ray is indicated to exclude other conditions affecting the area. May show calcification at the lower pole of knee cap bone or within the tendon in advance stage. USG and MRI both are equally effective in detecting the condition. Treatment consideration is rest, modification of activity, stretching and strengthening of thigh muscle, analgesic and icing. In non-resolving conditions USG guided infiltration of PRP is an effective treatment option. In a very advanced stage where there is disruption of the extensor mechanism or all the non-invasive treatments are exhausted then surgical debridement of the affected tendon with repair is recommended. This can be done both open or arthroscopically.
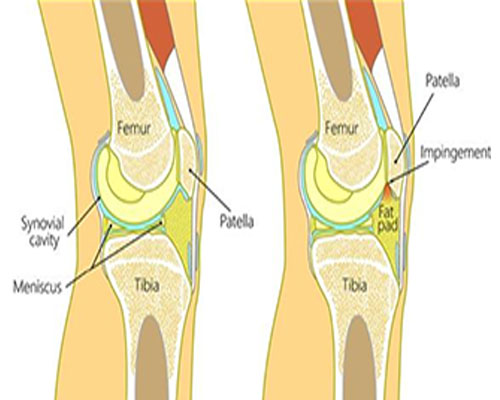
Hoffa’s syndrome
This is also known as infrapatellar fat pad syndrome. It affects the fat pad situated below the knee cap. This fat is situated outside the joint but between patellar tendon and joint. It acts as a shock absorber during different arcs of knee movement. Commonly the posterolateral part of the fat pad gets impinge between the knee cap and thigh bone when knee gets hyper extension, direct blow to anterior part of knee, altered movement due to any fibrosis of fat pad or other injury of the knee. The pain and tenderness is usually felt at either side of the patellar tendon. There may be some swelling around it. Pain starts following prolonged standing and hyperextension of the knee. Commonly seen in young women participating in jumping sports. Ligamentous laxity causing knee hyperextension is known to be a risk factor. MRI plays a key role in diagnosing the condition and exclusion of other causes of pain. Treatment includes rest, modification of activity, analgesic and icing. Local infiltration of steroids improves the symptom. Although it recovers but may take longer to improve. Rarely surgery is indicated for this condition.
Iliotibial Band Syndrome
It is a chronic overuse injury of the iliotibial band presented by pain and tenderness at the lateral aspect of the knee joint at the level of knee cap. It is often associated with weakness of hip abductor muscles. Overuse injury happens due to repeated flexion and extension of knee joints in cyclists and runners. Iliotibial band is a thick fibrous band on lateral aspect of thigh extending from waist bone crossing hip joint to lower leg bone just below knee joint. Area of iliotibial band at the level of the most prominent part of the lower end of the thigh bone is the impingement zone. Impingement happens at 300 of knee flexion when heel strikes the ground and pushes off during running, the stance phase. Iliotibial band remains in maximum taught situation at this point and knee also gets a varus thrust due to the body’s centre of gravity.
Pain is the sole symptom of IT band syndrome, which is activity related. Diagnosis is made from the history and local examination. Examination of hip and knee movement, spine deformity, pelvic tilt and knee deformity are assessed to identify any pre-existing risk factor. X-ray and MRI is done mainly to exclude other causes of anterolateral knee pain. MRI can also detect signal changes of the IT band around the impingement zone. Treatment for the acute stage is rest, activity modification, analgesic and icing. Physical rehabilitation in the form of IT band starching, posture correction, strengthening of hip, knee and core muscle plays a key role. Local infiltration with steroids and PRP can give symptomatic improvement. No surgical intervention is required for this condition.








